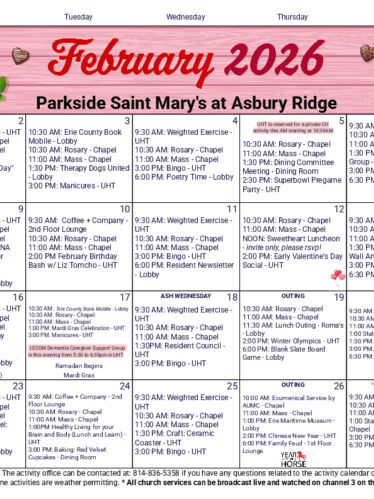
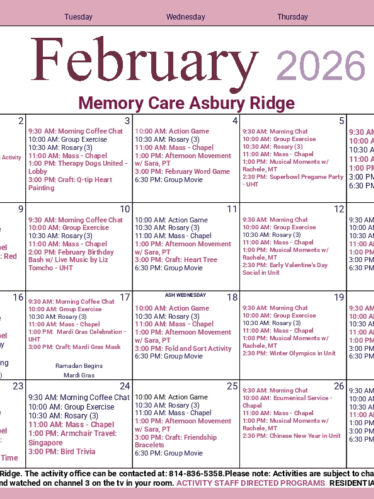
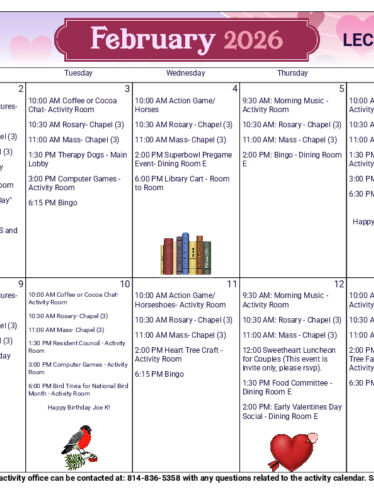
Activity Calendars
Resident activities are planned seven days-a-week by area of care. Activities are subject to change. If you have questions regarding the activity calendars, please contact our Activity Department at (814) 836-5358.
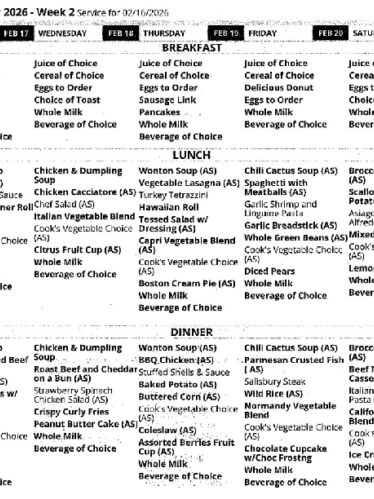
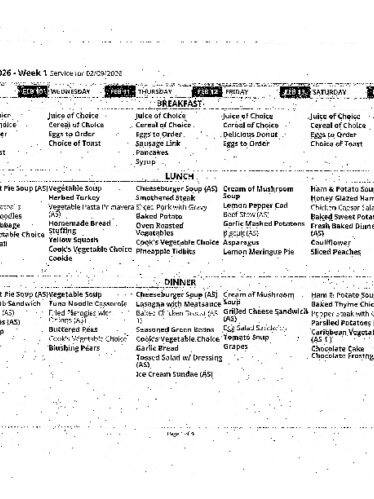
Dining Menu
Residents enjoy three meals a day in the Dining Rooms and have a variety of options at each meal to choose from. Menu's are provided weekly. These menu items are also available for visitors to purchase a la carte from St. Joe's Café during café operating hours. If you have questions regarding the menu or a residents meal options, please call the Dietary Department at (814) 836-5371.
What To Bring From Home
Deciding what to bring from home can be an overwhelming part of moving to a Retirement Community. Below is a checklist to help make your transition to Saint Mary's go as smooth as possible. These suggestions are offered as guidance. If you have questions regarding specific items allowed, please contact Social Services at (814) 836-5302.
A Glossary of Senior Living Terms
Ever heard someone use the abbreviation "SNF" or "ADL" and wonder what it stood for? You're not alone!
When transitioning to a senior living community, you are likely to come across new and unfamiliar terms. Use this brief glossary of senior living terms to better understand common terms, phrases and acronyms you might hear when talking with our team members and healthcare professionals.